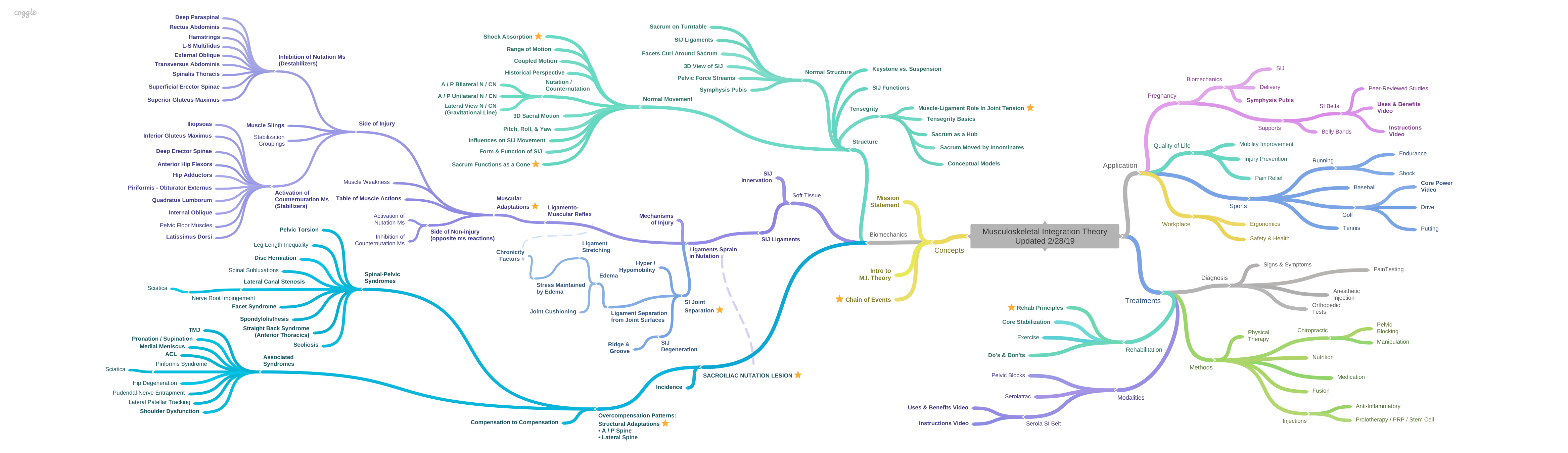
Sacroiliac Nutation Lesion Overview
Sacroiliac Joint Injury – Nutation Lesion Overview
The sacroiliac joint is the center of the motion, shock absorption, and weight transfer between the upper and lower body [1] (See Upper Body meets Lower Body). When force is transmitted superiorly or inferiorly through the body, a spring like action takes place. Upper body weight forces the sacral base anteriorly, while ground reaction forces the ilium to rotate posteriorly. (See The Gravitational Line). The sacroiliac joint is forced into nutation [2]p64-67 [3]p306. At the sacroiliac joint, this movement winds the interosseous ligament, drawing the sacrum and ilium closer [4] [5]p55, but not together [6] in a normal joint. Above the sacrum, the lumbar curve increases like a compressing spring [7]p54&60. The interosseous and associated ligaments, including the sacrospinous, sacrotuberous, anterior sacroiliac joint ligament, and the lower two bands of the iliolumbar ligament become stressed and tighten. (see Sacroiliac Ligaments). Once the energy is absorbed, and the end of range of motion is reached, the body reacts by going into counternutation, and all the above actions are reversed as the spring rebounds. In this sense, the sacroiliac ligaments that restrict nutation can be viewed as the central spring in shock absorption.
Ligaments Sprain in Nutation
When the force is greater than the ligaments can withstand, they sprain, and the joint goes past its normal endpoint. Failure of this mechanism to maintain ligamentous integrity is the weight-bearing sacroiliac joint injury, which I have named the Sacroiliac Nutation Syndrome. The central spring in the shock absorber system is damaged and the normal mechanism of force transference [8-10] becomes compromised (see SI Joint Separation).
Ligamento-Muscular Responses (See Ligamento-muscular Reflex).
Receptors in the ligaments respond selectively to activate or inhibit muscles to counter the stress applied to the injured ligaments [9, 11-16]. On the side of injury the ligamento-muscular reflex [17], activates the muscles that cause counternutation and inhibits the muscles that cause nutation, thus limiting the joint’s ability to move towards nutation and further damage the ligaments.
Muscles can do one of two things, increase or decrease contraction, as expressed through the speed of response, firing rate, strength, and duration. Muscular imbalance, as a result of ligament sprain, involves nociceptor and mechanoreceptor responses, positive feedback loops, delayed reaction times, weakness, and pain, which are expressed through altered structure and movement patterns. Additionally, due to poor blood supply, ligaments do not have the intrinsic ability to return to their normal length and heal, so the joint may remain hypermobile indefinitely [18].
In order to maintain stability in an injured joint, it must be kept within the normal range of motion; this can be accomplished by a brace or, to a lesser extent, by compensating muscular hyper or hypotonicity. One important key is realizing that these muscles are inhibited or tight for a reason – to protect the injured joint (see Basic Rehab Principles). Therefore, it is counterproductive to strengthen the inhibited muscles (which would induce nutation and stress the ligaments) or stretch the tight muscles (which would separate the joint surfaces and stress the ligaments), without first stabilizing the joint. But, with the sacroiliac joint, misconceptions regarding the interrelationship of ligaments and muscles, the shape and movement pattern of the sacroiliac joint itself, and other factors disguise many complications and contraindications that make treatment challenging. The entire concept of the Serola Theory is an attempt to clarify these misconceptions, help visualize the musculoskeletal system as a functioning whole, and enhance treatment options.
One aspect of movement in the body can be seen as shock absorption and rebound; in regard to the sacroiliac joint, they are respectively called nutation/counternutation, but their effects can be found anywhere in the musculoskeletal system, although they may have different names, e.g. foot pronation/supination, cervical & lumbar lordosis/kyphosis, thoracic kyphosis/lordosis, hip flexion/extension, elbow flexion/extension, even exhalation/inhalation, etc. It is better to visualize the whole body functioning as a unit in which all loads are shared by multiple joints and muscles (see Shock Absorption). With this perspective, when someone has an injury to any shock-absorbing joint, you can visualize the possibilities of other shock absorption mechanisms being compromised, and treat them as part of an interrelated unit. Since the core structure is the sacroiliac joint, stabilizing it should be a primary goal of treatment to the musculoskeletal system.
When considering the mechanisms of injury (See Mechanisms of Injury), it is not possible to indicate any single ligament as the one that is sprained. As expressed in the principles of tensegrity [19-22] (see Tensegrity), each ligament has a separate vector of support for the sacroiliac joint, but they all act together to provide an endpoint to its range of motion. Stress is distributed uniformly throughout the structure such that, whenever the joint goes past the normal range of motion, all ligaments that restrain the action are likely sprained as a unit.
Although most of the muscular mass of the body attaches to the sacrum and/or innominates (see Muscular Adaptations), muscular influence on the movement of these bones has long been disputed [23, 24] and never widely acknowledged. In fact, some anatomy books list the function of muscles that attach to the pelvis only by how they influence the extremities or spine, ignoring their effect on the pelvis. However, research has demonstrated that afferent information from the pelvic ligaments can influence muscle activation patterns to move the pelvis and lumbar spine [9]. Accordingly, the Serola Theory describes how individual muscles throughout the trunk, pelvis, and upper legs, acting through a combination of vectors dependent on their attachment points and angles of pull, move the sacroiliac joint through the patterns of nutation and counternutation. For this reason, I have classified them as nutators or counternutators. I have also provided illustrations and video images of many of the muscles, which demonstrate their actions (see Nutation Muscles) and (see Counternutation Muscles). The interplay between these two patterns governs all normal and dysfunctional musculoskeletal movement.
Although in the literature, far more attention is given to the articular area’s role in motion and dysfunction, some have suggested that the most significant dysfunction develops though sprain of the posterior ligamentous weight-bearing system [2, 6, 25-27], without suggesting the role of muscles in this system. The Serola Theory, recognizing the role of muscles, states that muscle splinting patterns occur principally for stabilization of the compromised weight-bearing system and that the movement patterns they generate are in line with the configuration of the synovial region of the joint.
Positioned at the center of shock absorption, the sacroiliac joint functions as a direct regulator of muscle tone for pelvic and trunk muscles and thereby influences posture and lumbar segmental stability [8] [9] [10] [28]. In its healthy state, the weight-bearing region of the sacroiliac joint is supported by balanced muscular action which ensures smoothly coordinated movement. However, upon injury to the ligamentous system, structural stabilization is then transferred to secondary systems. Muscular coordination is compromised for joint stability. As in all joints, ligament injuries in the sacroiliac joint can disrupt muscular response patterns and lead to spinal instability [28]. The muscles that attach to the bones that make up the joint will either contract to stabilize the joint or become inhibited to avoid furthering the injury. Knowing the difference can significantly influence treatment outcomes.
Ligament laxity allows increased separation of the sacral surface from the iliac surface [1] and weight bearing becomes compromised. The structural framework shifts to distribute gravitational and muscular forces in a manner that avoids overloading the injured ligaments [29]. Because most of the muscles from the head to the knees attach to either the sacrum or innominates, they become directly involved, and the effect is transferred throughout the kinematic chain. Because the lesion is almost always nutation, the response is almost always counternutation.
It is also important to note that the effect of a number of ligaments is cumulative; a group of ligaments is able to elicit a greater muscular response at much lower forces than a single ligament [30]. When one considers that the sacroiliac joint is supported by a vast network of ligaments, it is reasonable to assume that a sprain of the sacroiliac ligaments will cause considerable muscular reaction, even at low levels of stress [31], but especially during activity [13, 17]. Over time, the counternutation muscles on the lesioned side will become tight and painful [9, 32, 33]. Conversely, the muscles that promote ipsilateral nutation are inhibited and, over time, may become flaccid, atrophic and painful [34, 35]. The structure may be pulled into an altered movement pattern until the ligaments heal, which may be indefinitely [18].
With normal sacroiliac joints, when one side is in nutation, the opposite side is in counternutation, and muscular activity will match. Good examples of this reciprocating activity are gait [36] and cross-crawl patterning. However, with the nutation lesion, the coordination is disrupted as the muscles attempt to stabilize the sacroiliac joint. On the side of the sacroiliac joint injury, the counternutation muscles will become overactive and the nutation muscles will become inhibited to a similar degree. Conversely, on the contralateral side, the nutation muscles will become overactive and the counternutation muscles will become inhibited. This pattern will remain in an enhanced state as long as the joint remains unstable, and may worsen during periods of stress to the sacroiliac joint.
More commonly, both sides will have a nutation lesion, but one side will be the major injury. When this happens, depending on the severity of the lesion, varying degrees of contraction and inhibition will occur. When muscles are in a pattern of contraction, their antagonists are inhibited. Balanced exercise to both will lead to greater development of the contracted muscles and excessive tightness. As the imbalance between the tight counternutation and inhibited nutation muscles on the side of injury, and the added imbalance between side of injury and the normal, or less injured side, becomes magnified, the muscles may develop pain and structural distortion patterns that may cause more problems than the actual si joint injury. Other complicating factors may also influence muscle responses, such as patterns of use in work and lifestyle. For example, a massage therapist is more likely to develop shoulder and upper back symptoms, while a runner will be more likely to develop hip, leg, and foot symptoms.
In individuals with low back pain, the nutation muscles on the side of lesion are commonly hypotonic and painful, and the counternutation muscles are commonly tight and painful. The fact that similar patterns of muscle tightness and inhibition in the nutation lesion are both documented and predictable by other researchers, such as Jungmann [37] p21-23 and Janda [38] p97 [39]p480, strongly supports the concept of the Nutation Lesion Syndrome. The universality of these contraction/inhibition patterns provides a key to conceptualizing the integration of the musculoskeletal system, with the sacroiliac joint as the core.
Systemic Effects
As we look immediately superior and inferior to the pelvis, we see two additional significant shock absorber systems. The lumbosacral spine and hip form two highly flexible shock absorbing mechanisms which displace axial force considerably by transferring forces to the surrounding ligaments, muscles, and fascia through relatively large ranges of motion. But, when the system’s center, the interosseous and associated ligaments become sprained, the lumbosacral spine and hips stiffen to avoid transferring the shock to the sacroiliac joint. As a result, other shock absorbing mechanisms become overloaded and may degenerate and fail, including the foot, knee, hip, symphysis pubis, intervertebral disc, and shoulder [40]. Likewise, a lesion anywhere in the shock absorbing system may transfer additional stress to the sacroiliac joint and eventually lead to sacroiliac dysfunction.
Ligament injuries may be the major cause of chronic back pain [28]. Neural receptors within injured ligaments can disrupt muscular tone and timing and lead to spinal instability. The more ligaments involved, the greater the response, even at lower forces [30]. Considering that the sacroiliac joint is supported by a vast network of ligaments, it is reasonable to assume that a sprain of these ligaments will cause considerable muscular reaction and play a key role in many musculoskeletal disorders.
Neural and muscular reprogramming can disrupt muscular response patterns and lead to recurrent problems, including muscular spasm or inhibition, pain, weakness, joint instability, abnormal posture, disturbed motion patterns, altered gait, apprehension upon certain movements, delayed feed-forward activation, slowed reaction time, and giving way [9, 10, 18, 28, 32-34, 41-46] [35]p5-6. Eventually, poor balance and postural control may result in dysfunction and pain. In time, destructive cycles will develop as compensation patterns lead back to further the original injury (see Chronicity Factors). In the initial stages, the muscular imbalance may simply alter movement patterns but, over time, it may alter the structure, causing predictable patterns of dysfunction in posture and movement (see Overcompensation Patterns). Muscles distant to the pelvis can become involved, affecting distant joints.
In agreement with Johansson and Sojka’s hypothesis [12], Bullock-Saxton [47], Phillips [48], and Solomonow [49, 50] demonstrated that both sensory and motor changes are evident in muscles distant to the bones comprising an injured joint. Bullock-Saxton suggested that “…the arthrokinetic reflex might be considered as a triggering factor that would initiate a whole chain of adaptation reactions, eventually resulting in changed movement patterns” which are not limited to the side of injury, and could influence the uninjured side, as proposed by Lewit [51]p13 and Janda {Janda, 1978 #1235], Bullock-Saxton continued saying “Because muscles respond in different ways to peripheral injury, the results of this study suggest that the effects need to be sought in areas remote from the site of injury.” Because most of the muscles from the head to the knees attach to either the sacrum or innominates, they will become directly involved, thereby transferring the effect throughout the kinematic chain.
A sacroiliac sprain can change coordination patterns in many muscles which, by their attachments to the sacrum and pelvic bones, can act through various vectors and levers to alter posture and joint angles throughout the musculoskeletal system [9].These distortions can occur whether the muscles directly cross the sacroiliac joint, as in the knee, or do not directly cross the sacroiliac joint, as in the ankle [50, 52], or temporal mandibular joint [53].
In the model proposed by The Serola Theory, as a response to a right sacroiliac nutation lesion, the sacrum is pulled into some degree of counternutation on the right, indefinitely, unless the sacroiliac joint is properly stabilized and healed, which is extremely rare, but possible. Instead of healing, the body adapts; the pelvis will torque, the spine will twist, the extremities will rotate, and joints will move in asymmetrical patterns, etc. The effect can be seen distant to the sacroiliac joint and even on the opposite side. The structural alterations that develop eventually spread throughout the musculoskeletal system and forms the basis for many chronic dysfunctions, including those to the spine (see Spinal-Pelvic Syndromes) and extremities (see Associated Syndromes). Time and uneven contraction patterns produce chronic dysfunction.
To be Continued
From here, my work expands into the various aspects of the Sacroiliac Nutation Lesion; the effects on the sacroiliac and other joints, including normal and aberrant motion, degenerative changes, the ligamento-muscular relationships, tensegrity, compensatory muscular contraction/inhibition patterns, how it sets-up dysfunction in other joints, rehabilitation principles, diagnosis and treatment, as well as its applications in work and play of daily life.
References:
- Wilder, D.G., M.H. Pope, and J.W. Frymoyer, The functional topography of the sacroiliac joint. Spine, 1980. 5(6): p. 575-9.
- Kapandji, I.A., The Physiology of the Joints. Vol. 3. 1977: Churchill Livingstone.
- Neumann, D., Kinesiology of the Musculoskeletal System. Foundations for Physical Medicine. 2002: Mosby.
- Solonen, K.A., The sacroiliac joint in the light of anatomical, roentgenological and clinical studies. Acta Orthopaedica Scandinavica. Supplementum, 1957. 27(Suppl 27): p. 1-127.
- Vleeming, A., et al., The role of the sacroiliac joints in coupling between spine, pelvis, legs and arms., in Movement, Stability, and Low Back Pain, A. Vleeming, et al., Editors. 1997, Churchill Livingstone. p. 53-71.
- Vukicevic, S., et al., Holographic analysis of the human pelvis. Spine, 1991. 16(2): p. 209-14.
- Vleeming, A., et al., eds. Movement, Stability, & Low Back Pain. 1997, Churchill Livingstone.
- Snijders, C.J., Transfer of Lumbosacral Load to Iliac Bones and Legs: Part 1 – Biomechanics of Self-Bracing of the Sacroiliac Joints and its Significance for Treatment and Exercise. Clinical Biomechanics, 1993a. 8: p. 285-294.
- Indahl, A., et al., Sacroiliac joint involvement in activation of the porcine spinal and gluteal musculature. Journal of Spinal Disorders, 1999. 12(4): p. 325-30.
- Marshall, P. and B. Murphy, The effect of sacroiliac joint manipulation on feed-forward activation times of the deep abdominal musculature. Journal of Manipulative and Physiological Therapeutics, 2006. 29(3): p. 196-202.
- Kim, A.W., et al., Selective muscle activation following electrical stimulation of the collateral ligaments of the human knee joint. Archives of Physical Medicine and Rehabilitation, 1995. 76(8): p. 750-7.
- Johansson, H., Role of Knee Joint Ligaments in Proprioception and Regulation of Muscle Stiffness. Journal of Electromyography and Kinesiology, 1991. 1(3): p. 158-179.
- Raunest, J., M. Sager, and E. Burgener, Proprioceptive mechanisms in the cruciate ligaments: an electromyographic study on reflex activity in the thigh muscles. The Journal of Trauma, 1996. 41(3): p. 488-93.
- Stubbs, M., et al., Ligamento-muscular protective reflex in the lumbar spine of the feline. J Electromyogr Kinesiol, 1998. 8(4): p. 197-204.
- Solomonow, M., et al., The synergistic action of the anterior cruciate ligament and thigh muscles in maintaining joint stability. The American Journal of Sports Medicine, 1987. 15(3): p. 207-13.
- Tsuda, E., et al., Direct evidence of the anterior cruciate ligament-hamstring reflex arc in humans. The American journal of Sports Medicine, 2001. 29(1): p. 83-7.
- Palmer, I., Pathophysiology of the medial ligament of the knee joint. Acta Chirurgica Scandinavica, 1958. 115(4): p. 312-8.
- Kennedy, J.C., I.J. Alexander, and K.C. Hayes, Nerve supply of the human knee and its functional importance. The American Journal of Sports Medicine, 1982. 10(6): p. 329-35.
- Fuller, R.B., Synergetics. 1975, New York: McMillan.
- Levin, S.M., The Sacrum in Three-Dimensional Space. Spine: State of the Art Reviews, 1995. 9(2): p. 381-88.
- Levin, S.M., A different approach to the mechanics of the human pelvis: tensegrity, in Movement, Stability & Low Back Pain. The essential role of the pelvis., A. Vleeming, et al., Editors. 1997, Churchill Livinstone: New York. p. 157-167.
- Levin, S.M. The tensegrity system and pelvic pain syndrome. in Third World Congress on Low Back and Pelvic Pain. 1998. Vienna, Austria: EU Conference Organizers.
- Mitchell, F.L., Jr. and P.K.G. Mitchell, The Muscle Energy Manual. Vol. 3. 1999, East Lansing: MET Press.
- Bogduk, N., Clinical Anatomy of the Lumbar Spine and Sacrum. 2005: Elsevier Churchill Livingstone.
- DeJarnette, M., Sacral Occipital Technic Notes 1984. 1984: self published.
- DonTigny, R.L., Functional Biomechanics and Management of Pathomechanics of the Sacroiliac Joints. Spine: State of the Art Reviews, 1995. 9(2): p. 491-508.
- Cusi, M., SPECT-CT on patients with a clinical diagnosis of failure of load transfer of the sacro-iliac joint, in 7th Interdisciplinary World Congress on Low Back & Pelvic Pain. Effective Diagnosis and Treatment of Lumbopelvic Pain. 2010: Los Angeles, CA. p. 291-296.
- Panjabi, M.M., A hypothesis of chronic back pain: ligament subfailure injuries lead to muscle control dysfunction. European Spine Journal, 2006. 15(5): p. 668-76.
- van Dieen, J.H., J. Cholewicki, and A. Radebold, Trunk muscle recruitment patterns in patients with low back pain enhance the stability of the lumbar spine. Spine, 2003. 28(8): p. 834-41.
- Solomonow, M., et al., The ligamento-muscular stabilizing system of the spine. Spine, 1998. 23(23): p. 2552-62.
- Miyatsu, M., Y. Atsuta, and M. Watakabe, The physiology of mechanoreceptors in the anterior cruciate ligament. An experimental study in decerebrate-spinalised animals. The Journal of Bone and Joint Surgery. British volume, 1993. 75(4): p. 653-7.
- Indahl, A., et al., Interaction between the porcine lumbar intervertebral disc, zygapophysial joints, and paraspinal muscles. Spine, 1997. 22(24): p. 2834-40.
- Holm, S., A. Indahl, and M. Solomonow, Sensorimotor control of the spine. Journal of Electromyography Kinesiology, 2002. 12(3): p. 219-34.
- Baratta, R., et al., Muscular coactivation. The role of the antagonist musculature in maintaining knee stability. Am J Sports Med, 1988. 16(2): p. 113-22.
- Richardson, C., et al., Therapeutic Exercise for Spinal Segmental Stabilization in Low Back Pain. 1999: Churchill Livingstone.
- Gracovetsky, S. and H. Farfan, The optimum spine. Spine, 1984. 11(6): p. 543-73.
- Jungmann, M., The Jungmann Concept of Gravitational Strain Pathology. An Introductory View. 1977, New York, NY: Institute for Graviational Strain Pathology.
- Janda, V., Evaluation of Muscular Imbalance, in Rehabilitation of the Spine: A Practioner’s Manual, C. Liebenson, Editor. 1996, Williams & Wilkins. p. 97-112.
- Kuchera, M.L., Treatment of Graviational Strain Pathophysiology, in Movement, Stability, & Low Back Pain: The essential role of the pelvis, A. Vleeming, et al., Editors. 1997, Churchill Livinstone: New York. p. 477-99.
- Grieve, E.F., Mechanical dysfunction of the sacro-iliac joint. International Rehabilitation Medicine, 1983. 5(1): p. 46-52.
- Brand, R.A., A neurosensory hypothesis of ligament function. Medical Hypotheses, 1989. 29(4): p. 245-50.
- Lorentzon, R., et al., Thigh musculature in relation to chronic anterior cruciate ligament tear: muscle size, morphology, and mechanical output before reconstruction. The American Journal of Sports Medicine, 1989. 17(3): p. 423-9.
- Beard, D.J., et al., Proprioception after rupture of the anterior cruciate ligament. An objective indication of the need for surgery? J Bone Joint Surg Br, 1993. 75(2): p. 311-5.
- Richardson, C.A., et al., The relation between the transversus abdominis muscles, sacroiliac joint mechanics, and low back pain. Spine, 2002. 27(4): p. 399-405.
- Friemert, B., et al., Differentiation of hamstring short latency versus medium latency responses after tibia translation. Experimental Brain Research. Experimentelle Hirnforschung, 2005. 160(1): p. 1-9.
- Van der Wurff, P., E.J. Buijs, and G.J. Groen, Intensity mapping of pain referral areas in sacroiliac joint pain patients. Journal of Manipulative and Physiological Therapeutics, 2006. 29(3): p. 190-5.
- Freeman, M.A. and B. Wyke, Articular reflexes at the ankle joint: an electromyographic study of normal and abnormal influences of ankle-joint mechanoreceptors upon reflex activity in the leg muscles. The British Journal of Surgery, 1967. 54(12): p. 990-1001.
- Bullock-Saxton, J.E., Local sensation changes and altered hip muscle function following severe ankle sprain. Physical Therapy, 1994. 74(1): p. 17-28; discussion 28-31.
- Phillips, D., et al., Ligamentomuscular protective reflex in the elbow. The Journal of Hand Surgery. American volume., 1997. 22(3): p. 473-8.
- Solomonow, M. and M. Krogsgaard, Sensorimotor control of knee stability. A review. Scandinavian Journal of Medicine & Science in Sports, 2001. 11(2): p. 64-80.
- Solomonow, M., Ligaments: a source of work-related musculoskeletal disorders. Journal of Electromyography and Kinesiology, 2004. 14(1): p. 49-60.
- Lewit, K., Manipulative Therapy in Rehabilitation of the Locomotor System. 2nd ed. 1991, Oxford: Butterworth-Heinemann.
- Solomonow, M. and J. Lewis, Reflex from the ankle ligaments of the feline. Journal of Electromyography and Kinesiology, 2002. 12(3): p. 193-8.
- Standring, S., et al., eds. Gray’s Anatomy. 40th ed. 2008, Churchill Livingstone: London.