Rehab Principles
Central Model
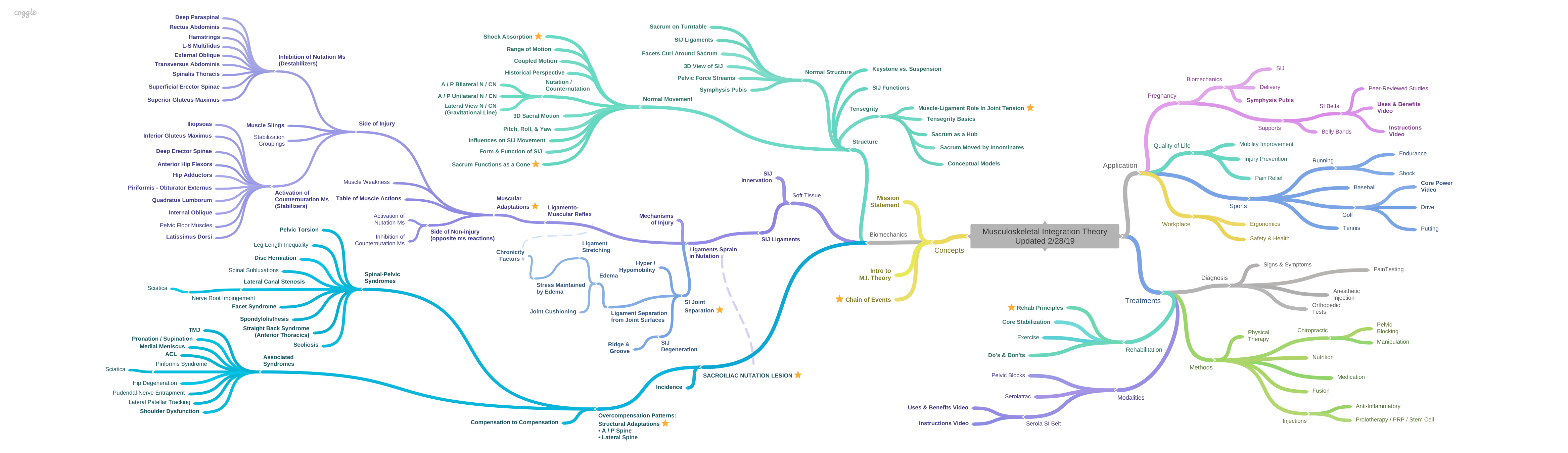
There are many misconceptions in the care of the musculoskeletal system because there is no central model of how things function together. Each area is looked at separately; foot, knee, hip, low back, shoulder, arm, neck, and head. There is no underlying model that ties them together as a functioning whole. Knowledge travels slowly and unevenly in the medical field, especially about the biomechanics of the musculoskeletal system. While some believe one thing, others may not know it is even possible.
With the sacroiliac joint (SIJ), misconceptions regarding the interrelationship of ligaments and muscles, the shape and movement pattern of the sacroiliac joint, and other factors disguise many complications and contraindications that make treatment challenging. The entire concept of the Serola Theory is an attempt to clarify these misconceptions and help visualize the musculoskeletal system as a functioning whole.
Ligament-muscle relationship (see Ligamento-muscular Reflex)
Bones are held together at the joints by ligaments. If the ligaments tear, even slightly, the bones separate to a proportionate degree. Instead of tearing in the middle, the interosseous sacroiliac ligament pulls away from its insertion into the joint surface. Within the ligaments, nerves activate a ligamento-muscular reflex, which tightens the muscles that would pull the joint together, and inhibit the muscles that would pull it apart. Eventually, both the tight and inhibited muscles become painful due to reduced circulation.
Our first inclination is to stretch the tight muscles. But, because the muscles are aligned to compress the sacroiliac joint, stretching them separates the joint surfaces, reinjuring the ligaments. The ligamento-muscular reflex, which causes the muscles to re-tighten, has a slow-acting reflex as a component that contributes to a great deal of confusion in the treatment program. So, as the patient goes through rehab, if treatments are frequent enough, the muscles don’t have enough time to re-tighten, so he/she appears to progress, as evidenced by less pain and increased mobility.
After a few weeks of treatment, or more, the patient feels good; the doctor is happy, the therapist is happy, and everyone is happy except the ligament, which is worse off than when treatment started, due to continuing microtrauma. Because the ligaments are the cause of the muscle tightness or inhibition of the antagonists, the pain and stiffness will return; the patient is prepared for this eventuality by being given exercises or stretches at home, and a positive destructive cycle is initiated.
So, what is the misconception? Our basic mistake is to think that relieving pain resolves the condition when, in reality, it may actually worsen the underlying injury, as evidenced by the slow-acting reflex producing continued muscle tightness after exercise or stretching has stopped. If treatment is frequent enough, the muscles may not get tight before the next treatment, so it will appear that progress is being made.
Pain Relief vs. Healing
In the musculoskeletal system, most pain relief comes through simply increasing circulation. But, healing comes through stabilizing the structure. Many things can increase circulation; massage, exercise, stretching, yoga, acupuncture, etc. and they may even be effective in realigning the structure to some degree. But, for the most part, these methods provide temporary pain relief and must be maintained regularly, or the pain and dysfunction will return and, with exercise and stretching, may return with greater intensity unless the sacroiliac joint is properly stabilized during those movements.
There are two components of stabilizing the sacroiliac joint (SIJ)
- Alignment (in order of increasing effectiveness)
- Exercise and stretching (best when SIJ is properly stabilized)
- Chiropractic Adjustment
- Prone Pelvic Blocking
- Compression (in order of increasing effectiveness)
- Strengthening nutators and, later, gradually adding counternutators
- Serola Sacroiliac Belt – the only belt designed to properly normalize the SIJ
- Supine Pelvic Blocking (aka Category II Blocking) – the only method that can heal the SIJ
Structural Goal
- Most of the pain & dysfunction is due to the compensation, not the original lesion
- The goal is to reverse the compensating counternutation pattern
- Bring the ilia posteriorly to neutral
- Decrease the posterior lumbosacral compression
- Increase the cervical and lumbar A/P curves
- De-rotate the externally rotated lower extremities and internally rotated upper extremities
- Bring sacroiliac syndesmosis surfaces together so ligaments can re-insert into the joint surfaces
Important Considerations
- The compensation that occurs in the weight-bearing Nutation Lesion is the activation of the muscles that stabilize the joint (Counternutators) and inhibition of the muscles that would further the injury (Nutators).
- Most of the pain & dysfunction is due to the compensation, not the original lesion
- We can only reverse the compensating structural patterns of counternutation (e.g. anterior pelvic tilt, lumbo-sacral compression, etc. by inducing nutation
- Drawback: by recreating nutation, we are recreating the original lesion
- The proprioceptive reaction (e.g. when bringing the ilia backward) is for the sacrum to go forward, opening the joint and re-stressing the ligaments
- To do this correctly, we must create a nutation pattern of the ilia without the nutation of the sacrum
- The Serola SI Belt ties the sacrum and ilium together so the ilium can pull the sacrum backward without reinjuring the ligaments, by maintaining normal range of motion
- Exercise and stretching must be specific and controlled
- Strengthen the muscles that promote nutation
- Stretch the muscles that promote counternutation
- Observe the Serola Sacroiliac Do’s and Don’ts at all times except while doing rehabilitation exercises and stretches
- Ligaments heal slowly. After 6 weeks, only 60%, and after 6 months only 80%, of pre-injury ligament strength in achieved under the best laboratory-controlled conditions. [1]
- Both the inhibited muscles and contracted muscles become painful because of reduced circulation due to decreased activity. With less pumping, less oxygen reaches the tissues and this leads to the release of chemical irritants, which build up and cause pain
- Treatment should be consistent until stability is achieved, and then monitored until the ligament heals (6 months to a year)
- Like any joint, the Nutation Lesion may recur if the SIJ undergoes significant trauma prior to healing, or at any stage in life, so remain aware of telltale pain patterns that are similar to what have been experienced while the Nutation Lesion was active
The ability of the ligaments and other connective tissue to undergo shortening when the joint surfaces are brought close together for an extended period of time (tissue creep) suggests that exercise/stretching and a pelvic belt should be used in rehabilitation of SIJ hypermobility [2-4].
The Serola SI Belt will hold the sacrum firmly to the ilia so that they are both brought back together without stressing the SIJ ligaments and without causing reactive muscle imbalance, yet it will allow normal range of motion at the sacroiliac joint.
You will notice that the recommended rehab exercises and stretches are almost exactly what I say not to do in my Do’s and Don’ts. The difference is that, in rehabilitation, we are trying to reverse the compensations in a controlled manner. Care must be taken to go gently while exercising and stretching and to always wear the Serola SI Belt.
At the end of the range of motion, it takes very little force to injure, or re-injure, the SI ligaments [5]. A doctor of chiropractic, medical/osteopathic doctor, or physical therapist, properly trained in the Serola Theory, will be able to develop an effective exercise and stretching routine and monitor the effects to see if you are doing them correctly and safely.
Usually, most of the pain is muscular, so the person usually finds relief by exercising and stretching. However, this approach can easily re-injure the joint, stress the ligaments, and re-activate the ligamento-muscular reflex. The muscles will tighten again once the exercise is stopped; it may take a day or weeks. Often, however, the individual will maintain a steady enough schedule of exercise that the muscles are continually cleansed of toxins and pain is minimal. This is the person who finds occasional stiffness that can be overcome with exercise and stretching. The average or debilitated person will find increased pain in the morning and some relief after moving around.
The lesion is excess nutation. Often, the compensation pattern, counternutation, is seen as the main cause of the patient’s complaints. He/she appears in a state of over-compensation: the hips are flexed (anterior pelvic tilt), the spine is straight above L3, with an increased lumbo-sacral angle, and the counternutating muscles are tight and painful (see Overcompensation Patterns).
Bodyweight keeps pushing the sacral base anterior and inferior. The iliac crest tries to close the gap, also rotating antero-inferiorly, chasing the sacrum in an attempt to reduce the nutation lesion. Likewise, other muscles attempt to pull the sacral base up and back to the ilia, eventually straightening the spine above L3. The nutating muscles contract about 23,000 times a day, against gravity, in their effort to rotate the sacrum and ilia towards each other.
The patient usually comes in suffering more from the compensation than from the actual lesion. The concept in rehabilitation is to reverse the counternutation compensation without re-injuring the nutation lesion.
Controlled Exercise vs. Free Motion
In a book called Therapeutic Exercise for Spinal Segmental Stabilization in Low Back Pain [6], the authors discussed their findings that certain trunk and pelvic muscles are inhibited and flaccid in most low back patients, resulting in reduced activation levels, reduced size, fatty infiltration, and greater fatigue and these changes remained after rigorous exercise regimens, even in elite athletes, even though pain decreased.
They describe a new method of exercise intended to stabilize the joints of the spine rather than simply strengthening the overall musculature. They introduced the idea that motion must be strictly limited or results would be poor; I believe that this was the beginning of core stabilization.
Previously, in most musculoskeletal pain syndromes, treatment plans were aimed at treating the muscles. However, stretching a tight muscle or strengthening an inhibited muscle may be counterproductive to joint stability. Appreciation of the ligamento-muscular reflex in our diagnosis and treatment regimens has been lacking, yet it embodies one of the most important concepts in understanding and correcting musculoskeletal pain and dysfunction.
Ligaments are regulators of muscle tone; when injured, they send signals to the muscles to either turn on or turn off, in order to protect the joint that contains the sprained ligaments. This is done by activating the muscles that would stabilize the SI joint and inhibiting the muscles that would destabilize it. In other words, the ligaments act to protect themselves and use the muscles to do it.
The functions of the muscles are modified to primarily guard the injured ligament. The nervous system must adopt a compensatory program that protects the joint during movement by altering muscle activation patterns and firing sequences. As a result, smooth power transmission will be disrupted, resulting in reduced power, endurance, and coordination.
If we look at the sacroiliac joint, we can get a better cause-and-effect relationship between excess movement and muscle inhibition affecting the core muscles. The key is to stabilize the joint and remove stress from the ligaments.
Core stabilization strategies are aimed at strengthening these inhibited muscles. But, these “core” muscles that promote nutation are inhibited for a reason; they make the sacroiliac lesion worse by bringing it into nutation, thereby re-stressing the ligaments. The counterintuitive aspect is that the popular concept of core stabilization correctly addresses the inhibited nutation muscles with exercises designed to strengthen them but disregards the effects of creating excess nutation at the sacroiliac joint.
Although exercise to the inhibited nutation muscles may result in a significant recovery of size and strength, they will revert to an atrophied state once treatment is stopped and some time passes. If core stabilization treatment is ongoing, it may appear that the patient is progressing because increased circulation will ease the pain and stiffness. However, the ligaments will be undergoing continued microtrauma, and the patient will regress once the treatment is stopped.
On the other hand, the counternutation muscles are tight to protect the joint by pulling it away from nutation. But, we mistakenly treat them by stretching, without stabilizing the SIJ, which brings the joint towards nutation and re-stresses the sprained ligaments, leading to greater instability. Although the tight counternutation muscles will become stretched and relax, they will tighten again due to the ligamento-muscular response.
Richardson and Jull [7] and Richardson, et al. [6] discuss findings that show that inhibition, weakness, and delayed onset of the transverse abdominis and multifidus, both nutators, play a significant role in low back pain. Based on their findings, they have developed an exercise program using the co-contraction of these muscles as the central part of a spinal stabilization program.
This concept is followed in some spinal stabilization regimens today: an inflatable pillow, with an attached gauge, is placed under the body; pressure changes will show if motion occurs. The person uses this knowledge to maintain a motionless spinal posture during exercise. The idea is to strengthen the muscles isometrically because the motion was found to be detrimental to the patient. With the proper perspective, we can see that these muscles, by inducing excess nutation, can worsen the sacroiliac joint nutation lesion, if they bring the structure past the normal range of motion; therefore, the joint is not brought to its end of the range of motion and the ligaments are not stressed. Although effective in reducing low back pain, these exercises demand precise control and concentration and must be done gently. Using this system, Hides [8] found an increase in the cross-sectional area of the involved multifidus. Although the program does reduce pain and decrease excess joint laxity, it is limited in how far it can take one beyond pain relief.
By considering the sacroiliac joint, we can see that as long as the motion they create doesn’t go past the normal range of motion of the sacroiliac joint, they won’t provoke an inhibitory response in the nutation muscles, so they will develop the increased function. In effect, their exercises attempt to reverse the compensatory counternutation pattern but extreme care is taken to avoid any but the most minimal movement.
Their concept is simple; controlled exercise directed at the weak, flaccid muscles in areas of dysfunction should help return stability to that area of the spine by increasing muscular compression. Although there is some validity to their program, they do not address the underlying mechanism that leads to dysfunction with motion, other than saying that it is most likely weak due to reflex inhibition. These muscles are inhibited and weak for a reason; it is very important to know that reason.
They recognized that more than a little motion would provoke a bad reaction but did not relate it to the correct spinal area. Although their concern was the stabilization of the lumbar spine, in effect, they were primarily stabilizing the sacroiliac joint.
The flaccid muscles which cause nutation, such as the multifidus and transversus abdominis, are part of a compensatory reaction to the weight-bearing nutation lesion of the sacroiliac joint. These nutating muscles are turned off through the ligamento-muscular reflex. Strengthening the muscles promoting nutation can easily cause the sacrum to go past the normal endpoint of nutation and into the lesion, stress the ligaments, re-injure the joint, and lead to more muscle tightness and inhibition. Yet, one must be able to safely induce nutation back to normal, short of re-creating the lesion; this is the idea and it is achievable.
The muscles that promote the nutation lesion (nutators) are inhibited and those that compensate are contracted (counternutators). The inhibited muscles are weak because they are inhibited. The tight muscles are weak because they are doing two things at once; stabilizing the joint and then performing their given task. Janda called it “tightness weakness.” All the muscles that attach to the innominate or sacrum are directly involved, which is most of the muscles in the body. Because such a large mass is directly involved, the effect is transferred throughout the body. This means that all, or at least most, of the muscles in the body are weaker if one has a Nutation Lesion. Of course, after stabilizing the Nutation Lesion, we may still have weak muscles from other causes, but they won’t be as widespread. The compensation pattern may have developed stress at other joints and set-up another self-perpetuating lesion; examples may be found in Associated Syndromes.
According to the authors, the essential first step in rehabilitation involved stabilizing the spine by isometric co-contraction of abdominal and low back muscles; in other words, keep the spine still while activating the inhibited muscles. The focus of the exercise is to control spinal position, rather than strength.
Once this stabilizing skill is learned, small advances are made in moving other parts of the body while preventing movement of the spine. This method of rehabilitation was very specific and controlled but it was difficult to do due to the patience and focus needed, and resulting in slow progress. It takes a trained doctor or therapist to teach and guide the patient in this technique.
But, somewhere along the line, spinal stabilization therapy advocates forgot about stabilizing the spine and just went for strengthening the muscles that were identified as necessary to stabilize the spine, which turned out to be nutation inducing muscles.
A new name was given to these muscles; core muscles. This “strengthen the core muscles” approach, without holding the spine motionless, contradicted the whole idea of spinal stabilization, from which it developed. As a result, core strengthening has become distorted into just strengthening the inhibited muscles, and then further degraded to just strengthening the trunk and pelvic muscles, with little-to-no regard to controlling movement.
Unfortunately, disregard for motion control may be the reason that, in some cases, core strengthening had no significant effects on low back pain in male or female athletes, although it did increase balance in left and right hip extensors [9].
In contrast, the Serola Belt, as endorsed in the Serola Theory, allows one to exercise with more power and movement by stabilizing the sacroiliac joint, in a sense, by acting as an external ligament. The nutation muscles may be strengthened and the counternutation muscles may be stretched relatively safely, but caution should still be taken to not overly stress the SI joint. Also, depending on the overall condition of one’s musculature, one should gradually add exercise to the counternutation muscles so that they are eventually balanced with the nutation muscles. It has been shown that it is important for opposing muscles to become balanced in order to create optimum joint stability [10].
Proprioception
Beard, Kyberd et al. [11] found that in the knee with an injured ACL, the hamstrings reacted significantly slower to sudden perturbations than in a normal knee. Also, a direct relationship was shown to exist between slowed reaction time and the frequency of ‘giving out’, which indicated that this functional instability may be due to a loss of proprioception. They suggested that the delayed response time in reflex hamstring contraction can be used as an objective measure of proprioception in the management of ACL deficiency.
Freeman, et al. [12] have demonstrated significantly improved proprioception in ankle joints after exercise programs that included balancing on boards with spheres on the under surface. The boards allowed full direction of motion, but did not allow an excess range of motion, and avoided re-injuring the ligaments.
Ligament Repair
Stubbs, Harris et al.[13] established the presence of a ligamento-muscular reflex from the mechanoreceptors in the lumbar supraspinous ligament to adjacent paraspinal muscles. Although done with electrical stimulation, they found that the contracted muscles, by creating an extension response, relieved tension on the ligament that would be strained by flexion, supports the theory of a ligamento-muscular protective reflex. They found the presence of types II and III mechanoreceptors. They suggested that type II (pacinian corpuscles) acted at low thresholds, monitored joint movement, and caused small adjustments in muscular activity for joint stability. Type III (golgi tendon-like endings) acted at high thresholds and created strong muscular responses to prevent injury and possible rupture, similar to the action of nociceptors, as described by Palmer[14], Peterson & Stener[15], Stener & Petersen, [16] and Ekholm & Eklund [17], above.
This study also emphasized that the importance of ligaments in sensory feedback to the muscles in stability of the spine, and other joints, should be considered in surgery. Ligaments should not be cut and replaced with non-neural tissue but rather repaired, if needed, and/or supported to promote rebalancing of proprioceptive input. Since the “injured ligament is likely to cause a persistently disturbed sensory feedback from the joint”, rehabilitation programs should address the muscle imbalances as well as strength.
Pregnancy
Ostgaard [18] studied 407 women during pregnancy and separated them into two categories, those with low back pain, which originated in the lumbar area, and those with posterior pelvic pain, which they defined as a concept not related to a specific structure but one that includes sacroiliac pain, sacroiliac syndrome, and pelvic pain. Either syndrome may have pain radiation down the posterior part of the thigh. Posterior pelvic pain was 4 times as common as lumbar back pain. They studied the response of these patients to two exercise programs and stated “Conclusively, (lumbar) back pain in pregnancy was reduced by subjective and objective measures in this study…but the large group of women with posterior pelvic pain were less fortunate in this aspect and remain the largest problem from the musculoskeletal system in pregnancy.” Women with posterior pelvic pain had higher intensity of pain than those with lumbar back pain after the exercise program. Importantly, women with lumbar back pain reduced the amount of sick leave, while women with posterior pelvic pain actually increased their time off work due to the exercise program.
Mens [19], studied the effects of exercise to the muscles that would appear to provide a bracing effect to the SI joint. The patients were women with pelvic pain who were at 6 weeks to 6 months post pregnancy. Muscles exercised were the Abdominal Obliques, Multifidus, Gluteus Maximus, and Latissimus Dorsi. They assumed that these muscles would help stabilize the SIJ because their lines of force were perpendicular to the surface of the sacroiliac joint. They were surprised that 25% of the participants had to stop training due to increased pain.
The sacroiliac joint must be stabilized properly and care must be taken not to force the joint beyond normal range of motion. In the study by [19], above, although the patients were given a sacroiliac belt, it was not stated whether the patients wore the belts during exercise or, if so, what type of belt was used. The main problem they had was during prone extension. Lying prone and lifting the straight leg causes such a strong nutation motion that excess motion it generates will aggravate the nutation lesion if the leg is lifted very far off the floor, regardless of which belt was used. Because they did not recognize that concept, they concluded that, in the patient group that they studied, exercise may be detrimental to the patient. They recommended that ergonomic advice and a sacroiliac belt were the best treatment. In most cases, exercise can, and should, be done wearing the Serola Sacroiliac Belt with consideration given to how strong of a nutation effect the exercise exerts. They further recommended that the concept of form and force closure should be revised – and that is what is happening in the Serola Theory.
Reflex Inhibition
Deandrade [20] stated “Muscle strengthening exercises should be used with caution when these result in reflex inhibition, to prevent further weakening. For example, it is futile to attempt to strengthen the quadriceps in the presence of a distended knee. Similarly, an inflamed joint should only be exercised within that range of movement that does not stimulate afferent inhibitory impulses.” With respect to the SIJ, this implies that we should be careful not to bring the joint past its normal range of motion or we could aggravate the sprained ligaments and re-activate the ligamento-muscular reflex, inducing additional spasm and inhibition; this should be a principle consideration in rehabilitation of any joint.
The Main Difference is Perspective
It is recognized that nutation brings the sacral and iliac surfaces towards each other, twisting and compacting the interosseous ligament. In a normal sacroiliac joint, nutation is considered to be the most stable position of the normal SIJ. Consequently, exercise programs are designed to promote nutation but without consideration to the idea that the ligaments restraining nutation are torn. Once injured, the sacroiliac joint can easily be forced past normal range of motion and further damage the ligaments; this is one of the main premises of the Serola Theory.
Joint Integrity for Muscular Balance
It is important to know if a particular exercise or stretch is detrimental to an individual; this can be easily tested by a one trained in the Serola Theory. Also, it should be emphasized that the balance to the musculature is one of the ultimate goals. There is a different point for each person where exercise and stretching should go from strengthening only the nutation muscles and stretching only the counternutation muscles to gradually add strengthening of the counternutation muscles and stretching of the nutation muscles. Within each person, this point may be different for each body area. For example, one may have more problems with the upper rather than the lower body and, therefore, may need to emphasize the upper nutation muscles longer than the lower nutation muscles before gradually including counternutation exercises, or vice versus. For this reason, I strongly recommend that rehabilitation programs be overseen by a chiropractor, medical doctor, or physical therapist that is well trained in the principles of the Serola Theory.
References:
- Gracovetsky, S. and H. Farfan, The optimum spine. Spine, 1984. 11(6): p. 543-73.
- Vleeming, A. Towards An Integrated Therapy For Peripartum Pelvic Instability-A study Of The Biomechanical Effects Of Pelvic Belts. in Proceedings of the 1st Interdisciplinary World Congress on Low Back Pain and its Relation to the Sacroiliac Joint. 1992.
- Snijders, C.J., et al., EMG recordings of abdominal and back muscles in various standing postures: validation of a biomechanical model on sacroiliac joint stability. Journal of Electromyography and Kinesiology, 1998. 8(4): p. 205-14.
- Harrison, D.E., D.D. Harrison, and S.J. Troyanovich, The sacroiliac joint: a review of anatomy and biomechanics with clinical implications. Journal of Manipulative Physiological Therapeutics, 1997. 20(9): p. 607-17.
- Grieve, E.F., Mechanical dysfunction of the sacro-iliac joint. International Rehabilitation Medicine, 1983. 5(1): p. 46-52.
- Richardson, C., et al., Therapeutic Exercise for Spinal Segmental Stabilization in Low Back Pain. 1999: Churchill Livingstone.
- Richardson, C.A. and G.A. Jull, Muscle control-pain control. What exercises would you prescribe? Man Ther, 1995. 1(1): p. 2-10.
- Hides, J.A., C.A. Richardson, and G.A. Jull, Multifidus muscle recovery is not automatic after resolution of acute, first-episode low back pain. Spine, 1996. 21(23): p. 2763-9.
- Nadler, S.F., et al., Hip muscle imbalance and low back pain in athletes: influence of core strengthening. Med Sci Sports Exerc, 2002. 34(1): p. 9-16.
- Baratta, R., et al., Muscular coactivation. The role of the antagonist musculature in maintaining knee stability. Am J Sports Med, 1988. 16(2): p. 113-22.
- Beard, D.J., et al., Proprioception after rupture of the anterior cruciate ligament. An objective indication of the need for surgery? J Bone Joint Surg Br, 1993. 75(2): p. 311-5.
- Freeman, M.A., M.R. Dean, and I.W. Hanham, The etiology and prevention of functional instability of the foot. J Bone Joint Surg Br, 1965. 47(4): p. 678-85.
- Stubbs, M., et al., Ligamento-muscular protective reflex in the lumbar spine of the feline. J Electromyogr Kinesiol, 1998. 8(4): p. 197-204.
- Palmer, I., Pathophysiology of the medial ligament of the knee joint. Acta Chirurgica Scandinavica, 1958. 115(4): p. 312-8.
- Petersen, I. and B. Stener, Experimental evaluation of the hypothesis of ligamento-muscular protective reflexes. III. A study in man using the medial collateral ligament of the knee joint. Acta Physiol Scand, 1959. 48(Suppl 166): p. 51-61.
- Stener, B. and I. Petersen, Electromyographic Investigation of Reflex Effects Upon Stretching the Partially Ruptured Medial Collateral Ligament of the Knee Joint. Acta Chirurgica Scandinavica, 1962. 124.
- Ekholm, J., G. Eklund, and S. Skoglund, On the reflex effects from the knee joint of the cat. Acta Physiologica Scandinavica, 1960. 50: p. 167-74.
- Ostgaard, H.C., et al., Reduction of back and posterior pelvic pain in pregnancy. Spine, 1994. 19(8): p. 894-900.
- Mens, J.M., C.J. Snijders, and H.J. Stam, Diagonal trunk muscle exercises in peripartum pelvic pain: a randomized clinical trial. Phys Ther, 2000. 80(12): p. 1164-73.
- Deandrade, J.R., C. Grant, and A.S. Dixon, Joint Distension and Reflex Muscle Inhibition in the Knee. The Journal of Bone and Joint Surgery. American volume, 1965. 47: p. 313-22.