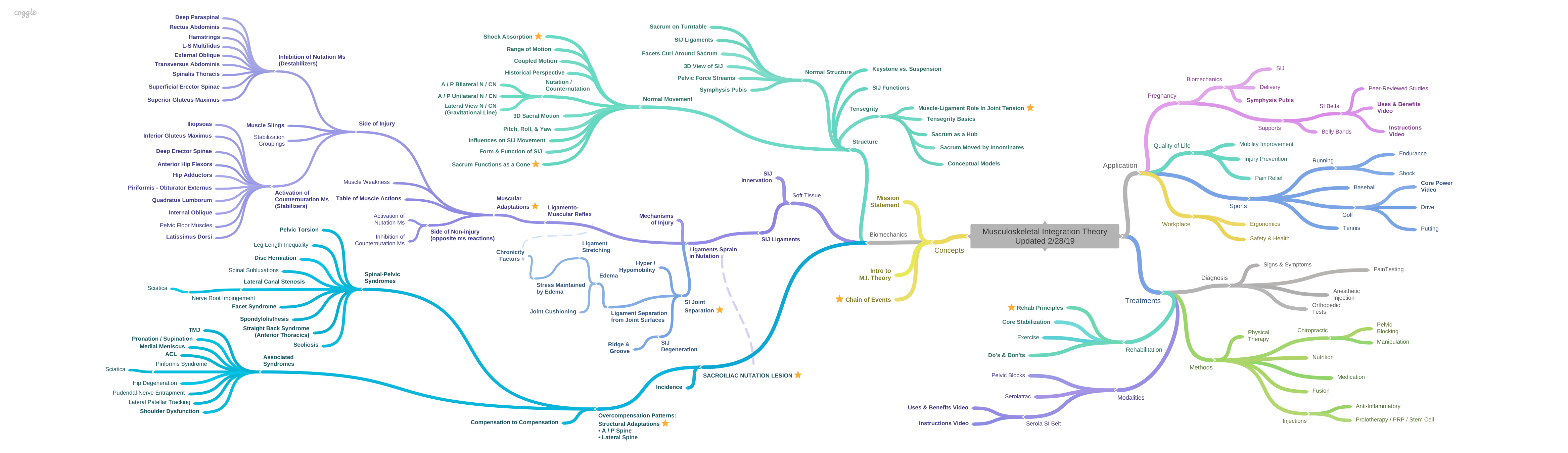
Introduction to Musculoskeletal Integration Theory
Historically, the sacroiliac joint was considered to be the main cause of back pain, as well as pelvic pain and sciatica. However, in 1934, the herniated lumbar disc was discovered to be a pain generating lesion, and disc herniation became the main focus of research into the mechanisms of back pain and sciatica. But, over time, the disc was found to be primary in only a limited number of back pain patients, and failed back surgeries have led to unsatisfactory outcomes in resolving back pain. More recently, with the advent of biomechanics, the past quarter century has seen the sacroiliac joint begin to regain acceptance as the main generator of not only SI joint pain, but also back, pelvic, and sciatic pain.
Unfortunately, sacroiliac joint pain is difficult to visualize with methods that are used to diagnose a herniated disc, especially x-rays and magnetic resonance imaging, due to its depth within the pelvis, and its complex configuration. Another problem is that scientific methods have been developed to visualize the lumbar disc as a static, non-moving picture, which can only point out the problem as it is captured at one instance in time. We can see a bulging disc and infer that it is touching a nerve, causing back pain. However, back pain is a result of dysfunction, which is not necessarily evident in a single moment. Rather, to get a better understanding of dysfunction, we must understand normal function and how the movement pattern that provides back, hip, or leg pain deviates in dysfunction; the key word being either function or dysfunction, which denotes action.
There are two different theories on how the sacroiliac joint functions, keystone (form closure) and suspensory. In the keystone concept, the sacrum is thought to compress into the ilia like a keystone in a Roman arch. In the suspensory concept, the sacrum is thought to be suspended from the ilia by strong ligaments. Although the suspensory concept was more popular historically, as of this writing, the keystone concept is more popular. Unfortunately, the currently popular concept involved with the return of the sacroiliac joint as the main cause of back, pelvic, and hip pain is misguided because it seeks to find stability in static posture. The proposition that the sacrum fits into the ilia, like a keystone in a Roman arch, may be influenced by the thought process that a static image could define function or dysfunction. It is like taking a picture of a person who has fallen and trying to imagine what caused him to fall, and what happened after he fell.
The keystone model developed out of the mistaken idea that the sacroiliac joint was immobile and stability was, therefore, a motionless state. The keystone concept leaves many known principles that cannot fit into the model as dead-ends, such as the ligamento-muscular reflex, muscular compensation patterns, mechanisms of injury, the effects of lumbo-pelvic traction on a keystone, SIJ biotensegrity, the shape of the sacral articular surfaces rounding out the sacral edges at the articular regions, misleading force streams allegedly perpendicular to the SIJ surface, joint tension, SIJ movement pattern with regards to a flat joint influencing 2D rotation about a transverse axis vs. a propeller shaped joint influencing 3D motion about an oblique axis, and whether nutation/counternutation – the movement of the core structure of the musculoskeletal system, the sacrum – has a role beyond the SIJ. Over the upcoming articles, currently in or approaching peer review, I hope to show you how the right perspective allows such inconsistencies to resolve into a unified model for our musculoskeletal system, based on the suspensory model.
Contrary to the idea that stability can be gained by jamming a wedge into supporting columns (stopping motion), modern analytical techniques have demonstrated that there is, in fact, a small amount of motion in the SIJ. Instead of revising the basic premise of a keystone, the concept was revised to a mobile keystone, in which the joint was more mobile (but less stable) as the sacrum pulled away from the wedge shaped receptacle formed by the ilia. In effect, this allowed one to take a small mental step from the static, immobile SIJ, and maintain a point of reference that stability is defined by reduced motion. Yet, it is widely known that, in biological systems, stability is defined as the ability to adapt to changes without a reduction in performance; to do this, a system must be able to move freely so it can distribute forces proportional to the incoming power and vector of the force. The wrist is an excellent example of dynamic stability; it can freely bend, twist, and rotate with considerable range of motion in order to transfer force streams. The pelvis is another example of dynamic stability which functions to transfer forces between the spine, sacroiliac joints, symphysis pubis, hips, and legs in smooth synchronous motion. Perhaps, the contradiction that presents when jamming bone into bone went unnoticed by proponents of the keystone model.
Function, or dysfunction, can best be defined by action; to do this, we must look at the movement patterns of the musculoskeletal system in both normal and dysfunctional joints and compare. Yet, the literature presents very little information on the movement pattern of the sacroiliac joint, other than it undergoes nutation and counternutation. But, even then, nutation is not taught well, if at all, in schools or post-graduate classes. Some teach that nutation involves only the sacrum, while others teach that it involves only the sacrum and ilium, but none teach that it involves anything outside of the pelvis. In my articles, we will be able to understand how nutation and counternutation are the core movement patterns that extend outward to the rest of the musculoskeletal system; this serves as a solid basis for understanding normal and dysfunctional movement patterns. Next, we will investigate the ligaments and muscles that help stabilize and provide movement throughout the musculoskeletal system within the context of nutation and counternutation.
Ligaments, being basically non-contractile, are the primary stabilizers of a joint, preventing excess motion but allowing motion within a specific range. As such, ligament injury should have prime consideration in diagnosis of joint dysfunction. Also, because the muscles generate movement, they must also have prime consideration in diagnosis of dysfunction generating back, pelvic, or leg pain. Muscles help create stability and transfer loads by reacting to signals from the ligaments via the arthrokinetic reflex. However, when these ligaments are sprained, nerves within them stimulate, or inhibit, specific muscles to keep pressure off the injured ligament. This reaction is known as the ligamento-muscular reflex. The functions of the muscles are modified to guard the injured ligament, altering joint function.
Instead of significant friction between two surfaces pressing together, ligamentous suspension provides a relatively frictionless method of pulling the sacrum through its range of motion. Pivoting rotary action provides a continuum of movement in which force blends seamlessly between the trunk and contralateral lower extremity, with the sacrum as the core structure of an integrated system. As a tensegrity structure, it allows distribution of force throughout the body in both load absorption and muscular propulsion, in which muscles, ligaments, and other connective tissues play a significant role.
To diagnose joint dysfunction, it is reasonable that we look at activity of the surrounding structures, rather than an image of a structure at a particular moment in time; this may be difficult for some to accept since we have to develop a different mind-set and a different paradigm. But, the current model is clearly not working as back, pelvic, and leg pain remain a mystery. The answer is simple to understand once we look in the right direction.
To maintain stability after injury, the nervous system must adopt a compensatory program that protects the joint during movement by altering muscle activation patterns and firing sequences to redirect force vectors. As a result, smooth power transmission will be disrupted, resulting in reduced power, endurance, and coordination. We can measure movement, muscle strength, tonicity, endurance and line of action, which gives us the ability to analyze function, diagnose a dysfunctional joint and lead to greater understanding of their influence on back, pelvic, and leg pain. New insights into the interrelationship of muscle and ligament should influence our treatment options.